
NGL | EssentialLTC – Long Term Care Awareness Month
NGL is dedicated to helping you get the most out of Long Term Care Awareness Month. We have the consumer materials you need to help you increase your client’s knowledge of this month. Click the links below to download a PDF version of the material.
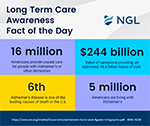
Downloadable Social Media Posts
There are 14 different social media infographics you can use on your social media platforms to inform your customers why they should consider long-term care planning. Click here to download the posts.

Consumer Brochure*
This brochure can help you comprehensively explain the benefits of this crucial insurance to your clients. It takes consumers through why long-term care is important, payment options, product features, and optional benefit features. Click here to download a PDF copy.

Consumer Presentation*
We’ve taken our Consumer Brochure and made it into a presentation that you can show your clients! It gives a high-level breakdown of why LTC insurance is so important. Click here for a PDF version.

Consumer Flyer*
Perfect for a handout or a leave-behind, the Consumer Flyer is a quick way to introduce the concept of LTC and NGL as a company. Click here to download a PDF of the flyer.
Employer Brochure*
Like the Consumer Flyer, the Employer Brochure is a great introduction to how NGL EssentialLTC can benefit employers. Click here to download a PDF of the brochure.

Claims Flyer
This step-by-step flyer is a great tool to help you explain the NGL EssentialLTC claims process to your clients. It lays out eligibility for claims and the steps your clients can expect when filing for benefits. Click here to download a PDF of the flyer.
For agent inquiries contact your dedicated Agent Services Team at 1 (888) 505.2332 or status@ngl-essentialltc.com. For sales questions contact the Long-Term Care Sales Team at LTC@nglic.com.
*Available for use in AK, AL, AR, CO, GA, IA, ID, IL, KS, KY, LA, MA, MD, ME, MI, MN, MO, MS, NC, NE, NH, NM, NV, OH, OK, OR, PA, RI, SC, TN, TX, UT, VA, VT, WA, WI, WV, WY.
Check the Agent Resource Center for versions available for AZ, CA, CT, DC, DE, FL, HI, IN, ND, NJ, SD.
1 (800) 772-6881 x7731 | sales@pfsinsurance.com
Contact a Pinnacle Representative if you have any questions.
1 (800) 772-6881
support@pfsinsurance.com









