Humana | Assisting Members impacted by loss of Medicaid Status
March 17, 2023
Medicaid Redetermination:
Assisting Members impacted by the loss of Medicaid Status

What you should know
- Annual Medicaid redetermination was paused during the Public Health Emergency (PHE)
- February 1, states can begin their Medicaid Redetermination Process, with the potential for Medicaid disenrollment to start April 1, 2023
- Each state determines when its redetermination process will begin
- Impacted beneficiaries will be notified by the state approximately 60 calendar days prior to their disenrollment effective date from State Medicaid
What this means for you
- You can prepare for Dual Eligible Members to complete the redetermination process for continued Medicaid Coverage
- Dual Eligible Special Needs Plan (DSNP) members, who are found to be ineligible for Medicaid coverage, will need Agent assistance to obtain new coverage and maintain continuity of care
- Non-DSNP members, whose eligibility level changes, may also require a plan review to ensure they’re still on the plan best suited for them
Please remind impacted DSNP members of the following:
- Confirm contact information is up to date with the state
- Watch for a mail from the state requesting additional documentation
- Respond to any request from the state promptly and within the deadlines
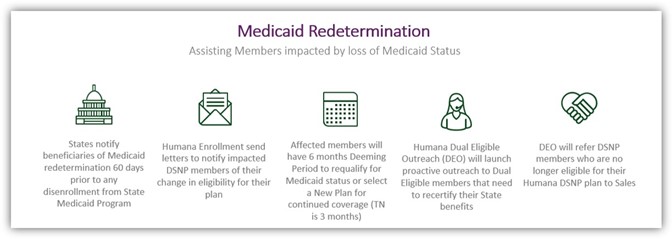
Process at a glance
Where to learn more
- Visit Ignite for a dedicated resource document to help assist agents with supporting members who may be at risk of losing their Medicaid coverage.
For more information, contact a Pinnacle Financial Services representative today
1 (800) 772-6881 x7731 | sales@pfsinsurance.com
“
Contact a Pinnacle Representative if you have any questions.
1 (800) 772-6881
support@pfsinsurance.com

0 Comments